Have you ever wondered why certain foods leave you feeling uncomfortably bloated, gassy, or in digestive distress whilst others don’t? If you’ve experienced these symptoms, particularly after eating foods like onions, wheat, or dairy, you may be sensitive to a group of carbohydrates known as FODMAPs. Understanding exactly how these compounds trigger gas and bloating can transform the way you approach your meals and help you regain control over your digestive comfort. This article will guide you through the biological mechanisms behind FODMAP intolerance, explain why some people are more sensitive than others, and provide practical strategies for identifying whether FODMAPs are the culprits behind your symptoms.
What Are FODMAPs and Why Do They Matter?
FODMAPs is an acronym that stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides And Polyols. These are specific types of short-chain carbohydrates that share two important characteristics: they are poorly absorbed in the small intestine, and they are rapidly fermented by gut bacteria. Whilst these compounds are found naturally in many nutritious foods, they can cause significant digestive symptoms in sensitive individuals.
The five categories of FODMAPs each include different types of carbohydrates. Oligosaccharides include fructans (found in wheat, onions, and garlic) and galacto-oligosaccharides or GOS (found in legumes). Disaccharides primarily refer to lactose, the sugar in dairy products. Monosaccharides include excess fructose found in honey, apples, and high-fructose corn syrup. Polyols are sugar alcohols like sorbitol and mannitol, found in some fruits and artificial sweeteners.
For most people, FODMAPs pass through the digestive system without causing issues. However, individuals with IBS symptoms or other digestive sensitivities often experience uncomfortable reactions. Understanding the mechanisms behind these reactions is essential for managing digestive symptoms effectively and making informed dietary choices.
How FODMAPs Trigger Fermentation in Your Gut
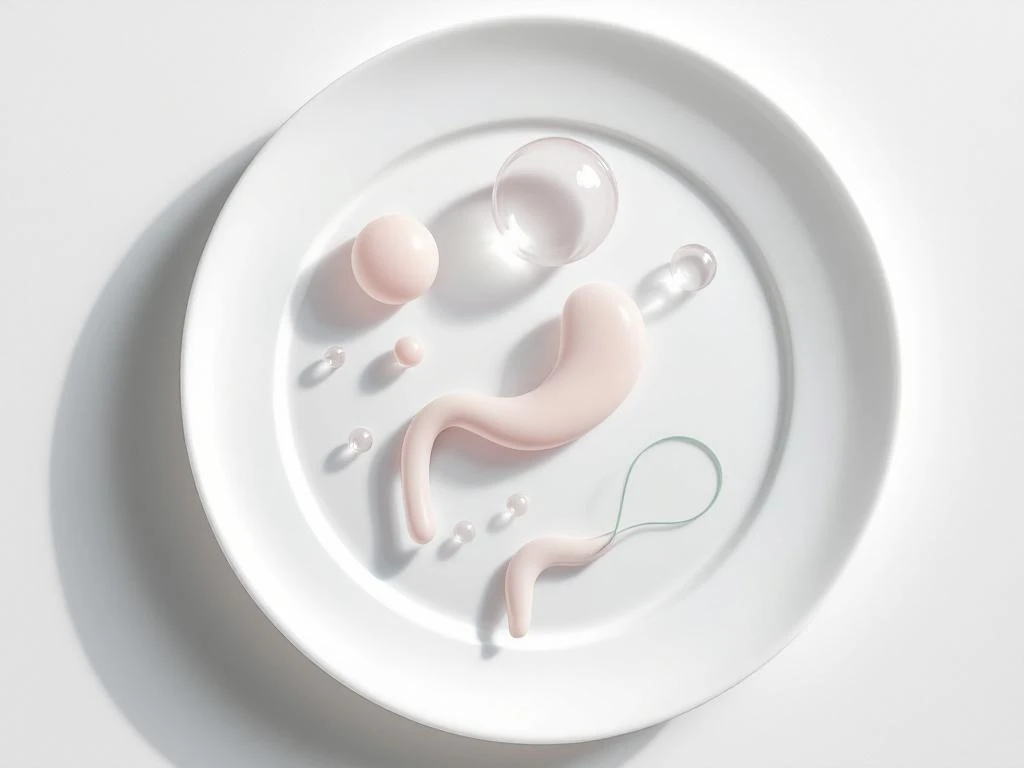
When you eat foods containing FODMAPs, these carbohydrates travel through your digestive tract. Unlike other nutrients that are absorbed efficiently in the small intestine, FODMAPs largely pass through undigested, eventually reaching your large intestine (colon). This is where the trouble begins for sensitive individuals.
Your large intestine is home to trillions of gut bacteria that form your gut microbiome. These microorganisms thrive on carbohydrates, and when FODMAPs arrive, they eagerly begin breaking them down through a process called fermentation. Whilst fermentation is a normal and even beneficial process in many cases, it produces gases as byproducts, primarily hydrogen, methane, and carbon dioxide.
The gas produced during FODMAP fermentation doesn’t simply disappear—it accumulates in your intestines, causing the characteristic bloating, distension, and discomfort that many people with FODMAP intolerance experience.
The speed and extent of this fermentation process can vary depending on which types of FODMAPs you’ve consumed and the composition of your gut microbiome. Some FODMAPs ferment more rapidly than others, leading to quicker symptom onset. The volume of gas produced can stretch your intestinal walls, triggering pain receptors and creating that uncomfortable feeling of fullness and pressure. For individuals with heightened sensitivity, even normal amounts of gas can feel overwhelming.
Why FODMAPs Draw Water Into Your Intestines
Beyond fermentation, FODMAPs cause digestive distress through a second mechanism called the osmotic effect. Because these carbohydrates are small molecules that remain unabsorbed in your digestive tract, they create an osmotic gradient that pulls water from your body into your intestines.
Think of it like this: when there’s a high concentration of dissolved particles (FODMAPs) in your gut, your body attempts to balance this concentration by drawing water into the intestinal space. This increased fluid volume can lead to several uncomfortable symptoms. The extra water can cause your intestines to stretch and distend, contributing to bloating and that heavy, uncomfortable feeling in your abdomen.
The osmotic effect also explains why many people with FODMAP intolerance experience changes in their bowel movements after consuming high-FODMAP foods. The increased water content can lead to looser stools or diarrhoea, whilst in some individuals, the combination of gas and fluid can paradoxically slow transit time, leading to constipation. The scientific foundation of the low FODMAP diet is built on understanding these dual mechanisms of fermentation and osmotic effects.
The severity of the osmotic effect varies depending on which FODMAPs you’ve consumed. Polyols, for example, are particularly known for their strong osmotic properties, which is why sugar-free products containing these sweeteners often carry warnings about potential laxative effects.
What Makes Some People Sensitive to FODMAPs?
If FODMAPs are present in so many common foods, why don’t they cause problems for everyone? The answer lies in individual differences in digestive function and gut characteristics. Several factors determine whether you’ll experience symptoms from FODMAPs.
Gut motility, the speed at which food moves through your digestive system, plays a significant role. People with slower gut motility give bacteria more time to ferment FODMAPs, potentially producing more gas. Conversely, rapid motility may not allow enough time for proper absorption of other nutrients, but can sometimes reduce fermentation time.
Visceral hypersensitivity is another crucial factor. This refers to heightened sensitivity of the nerves in your gut wall. Even normal amounts of gas or stretching that wouldn’t bother most people can trigger significant pain and discomfort in individuals with visceral hypersensitivity. This condition is particularly common in people with IBS symptoms.
Your unique gut microbiome composition also influences FODMAP sensitivity. The types and quantities of bacteria residing in your intestines determine how efficiently FODMAPs are fermented and what byproducts are produced. Some bacterial profiles may generate more gas or produce different types of gases that cause more discomfort.
Conditions like irritable bowel syndrome create an environment where all these factors converge. IBS often involves altered gut motility, visceral hypersensitivity, and changes in gut microbiome composition, making individuals with this condition particularly susceptible to FODMAP-related symptoms. Other factors such as stress, previous gastrointestinal infections, and inflammation can also increase FODMAP sensitivity.
How to Identify if FODMAPs Are Causing Your Symptoms
Recognising whether FODMAPs are behind your digestive symptoms requires careful attention to patterns and timing. FODMAP-related symptoms typically appear within a few hours of eating trigger foods, though the exact timing can vary. Common symptoms include bloating, abdominal pain or cramping, excessive gas, diarrhoea, constipation, or alternating between both.
Pay attention to when your symptoms occur in relation to meals. Do you notice discomfort after eating wheat-based pasta or bread? Does your stomach bloat after consuming dairy products or certain fruits? Keeping a food and symptom diary can reveal patterns that might otherwise go unnoticed.
The gold standard approach for identifying FODMAP intolerance is the low FODMAP diet protocol, which involves three distinct phases. During the elimination phase, you temporarily remove high-FODMAP foods from your diet for several weeks, allowing your digestive system to settle and symptoms to improve. This phase helps establish whether FODMAPs are indeed contributing to your discomfort.
The reintroduction phase follows, where you systematically test individual FODMAP groups one at a time to identify your specific triggers. Not everyone reacts to all FODMAPs, and this phase helps you understand your personal tolerance levels. The final personalisation phase involves creating a long-term eating pattern that avoids your specific triggers whilst including as many foods as possible for nutritional variety.
It’s worth noting that symptom severity can depend on portion sizes and FODMAP load. You might tolerate small amounts of certain high-FODMAP foods but experience symptoms with larger portions. Additionally, the cumulative effect matters—eating multiple moderate-FODMAP foods in one meal might trigger symptoms even if each food individually would be tolerable.
If you suspect FODMAPs are causing your gas and bloating, consider working with a registered dietitian who specialises in digestive health. They can guide you through the elimination and reintroduction process properly, ensuring you maintain adequate nutrition whilst identifying your triggers. Self-diagnosis and long-term restriction without proper guidance can lead to nutritional deficiencies and unnecessarily limited food choices.
Understanding the mechanisms behind FODMAP intolerance empowers you to make informed decisions about your diet and digestive health. By recognising how fermentation and osmotic effects create symptoms, identifying your personal sensitivity factors, and systematically testing your tolerance, you can develop a sustainable approach to eating that minimises discomfort whilst maximising nutritional variety and enjoyment.