The low FODMAP diet is a therapeutic eating approach that reduces specific types of carbohydrates to manage digestive symptoms, particularly in people with irritable bowel syndrome (IBS). It works by temporarily eliminating foods containing fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, which can trigger bloating, pain, and other gut issues. This structured three-phase process helps identify personal food triggers whilst maintaining nutritional balance.
What is the low FODMAP diet and why was it developed?
The low FODMAP diet is a science-based eating plan designed to manage symptoms of IBS and other functional digestive disorders. FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols, which are types of short-chain carbohydrates that some people struggle to digest properly.
Researchers at Monash University in Australia developed this approach after discovering that these specific carbohydrates could trigger digestive symptoms in sensitive individuals. Their groundbreaking work provided the first systematic method for identifying which foods cause problems and which don’t.
The fundamental principle is straightforward: certain short-chain carbohydrates pass through the small intestine without being properly absorbed. When they reach the large intestine, gut bacteria ferment them rapidly, producing gas and other byproducts that cause discomfort in people with sensitive digestive systems.
This diet isn’t meant to be a permanent lifestyle change. Rather, it’s a diagnostic tool that helps you understand your body’s unique responses to different foods, allowing you to create a personalized eating plan that minimizes symptoms whilst maximizing food variety.
How does the low FODMAP diet actually work in your digestive system?
FODMAPs affect your gut through two main mechanisms: osmosis and fermentation. When these carbohydrates aren’t absorbed in the small intestine, they draw water into the digestive tract through osmosis, which can lead to diarrhea and loose stools in sensitive individuals.
Once FODMAPs reach the large intestine, gut bacteria rapidly ferment them. This fermentation process produces gases (hydrogen, methane, and carbon dioxide) that cause bloating, distension, and abdominal pain. In people with IBS, the gut is often more sensitive to this stretching, making even normal amounts of gas feel uncomfortable.
The combination of excess water and gas in the intestines creates the classic IBS symptoms: bloating, cramping, altered bowel movements, and general digestive discomfort. By reducing FODMAP intake, you minimize both the osmotic effect and the fermentation process.
When you follow a low FODMAP diet, your digestive system experiences less stretching and irritation. This gives your gut a chance to settle down, reducing inflammation and hypersensitivity. Many people notice their symptoms improve within a few weeks as their digestive system calms.
What are the three phases of the low FODMAP diet?
The low FODMAP diet works through three distinct phases, each serving a specific purpose. The elimination phase typically lasts 2 to 6 weeks, during which you strictly avoid high FODMAP foods. This phase allows your symptoms to settle and establishes a baseline of improved digestive comfort.
During elimination, you’ll eat only low FODMAP foods from each food group. This isn’t about deprivation but rather creating a calm digestive environment. Most people notice significant symptom improvement during this phase, which confirms whether FODMAPs are indeed triggering their issues.
The reintroduction phase is where the real detective work happens. You systematically test different FODMAP groups (one at a time) to identify which specific types trigger your symptoms. This phase usually takes 6 to 8 weeks and requires careful attention to how your body responds to each food challenge.
The final personalization phase is your long-term eating plan based on what you learned during reintroduction. You’ll include all the FODMAPs you tolerate well whilst avoiding or limiting only those that genuinely cause problems. This phase ensures you eat the most varied diet possible whilst keeping symptoms under control.
Which foods are high in FODMAPs and what should you avoid?
High FODMAP fruits include apples, pears, watermelon, mangoes, cherries, and stone fruits. These contain excess fructose or polyols that can trigger symptoms. Vegetables like onions, garlic, cauliflower, mushrooms, and asparagus are also high in FODMAPs and commonly cause issues.
Wheat and rye products contain fructans and oligosaccharides, making regular bread, pasta, and cereals problematic during the elimination phase. Legumes (beans, lentils, chickpeas) are high in galacto-oligosaccharides, another FODMAP type that causes fermentation.
Dairy products containing lactose (milk, soft cheeses, yoghurt, ice cream) can trigger symptoms in people sensitive to this disaccharide. Even small amounts of regular milk can cause issues for some individuals.
Portion sizes matter significantly with FODMAPs. A small serving of a high FODMAP food might be tolerable, whilst a large serving causes symptoms. This is why the reintroduction phase tests different quantities to find your personal threshold for each food.
What can you eat on the low FODMAP diet?
You can enjoy a wide variety of proteins including all fresh meat, poultry, fish, eggs, and firm tofu. These foods are naturally low in FODMAPs and form the foundation of satisfying meals. At SimpleHomechef, we create recipes that showcase how delicious low FODMAP eating can be.
Grains like rice, quinoa, oats, and gluten-free bread provide excellent alternatives to wheat-based products. Potatoes, both regular and sweet, are perfectly safe and wonderfully versatile for any meal.
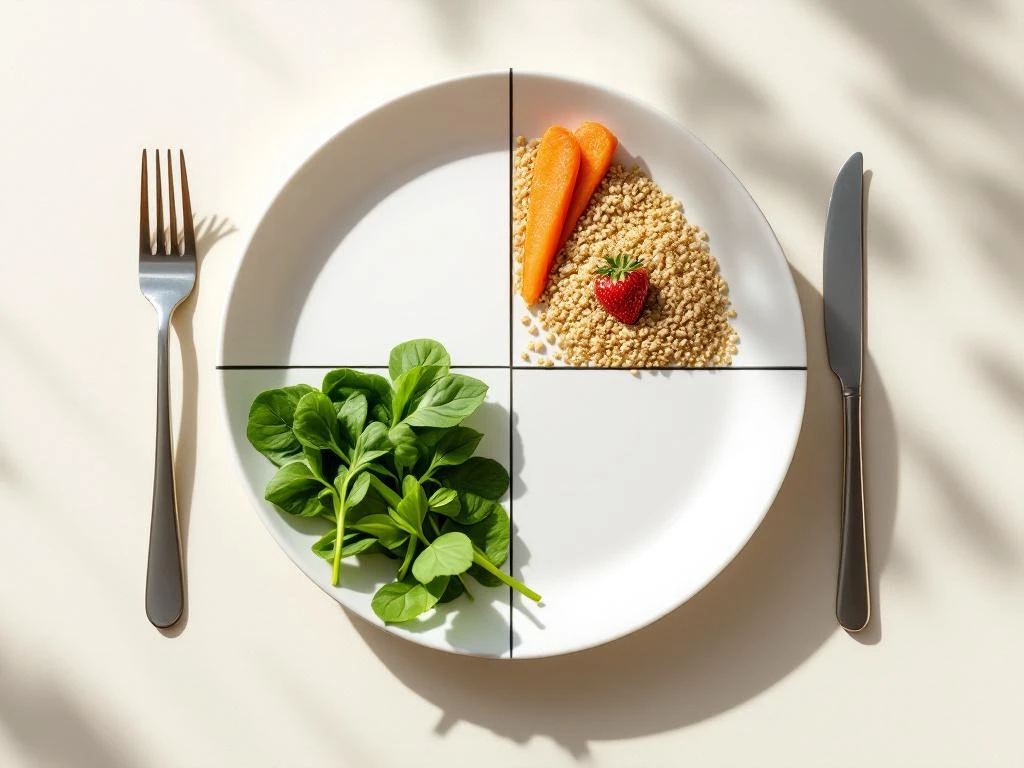
Low FODMAP fruits include bananas, oranges, strawberries, blueberries, grapes, and kiwi fruit. These provide natural sweetness and essential nutrients without triggering symptoms. Vegetables such as carrots, spinach, courgettes, peppers, tomatoes, and green beans offer plenty of variety and nutrition.
Lactose-free dairy products, hard cheeses, and plant-based alternatives (like almond milk) allow you to enjoy creamy textures and calcium-rich options. The key is that you’re not restricted to bland, boring meals but rather learning which of the many delicious options work best for your body.
How long does it take to see results from the low FODMAP diet?
Most people notice symptom improvement within 2 to 6 weeks of starting the elimination phase. Some individuals feel better within days, whilst others need the full 6 weeks to experience significant relief. This variation is normal and depends on your individual sensitivity and symptom severity.
The speed of improvement often relates to how strictly you follow the diet and how severe your symptoms were initially. People with mild symptoms might notice subtle changes, whilst those with severe IBS often experience dramatic relief once they’ve eliminated their trigger foods.
Several factors influence your response time: the accuracy of your FODMAP food choices, your overall gut health, stress levels, and whether FODMAPs are indeed your primary trigger. Some people have additional issues (like stress-related IBS or other food intolerances) that affect results.
If you haven’t noticed improvement after 6 weeks of careful elimination, it’s worth consulting with a healthcare professional. FODMAPs might not be your main trigger, or you might be inadvertently consuming high FODMAP foods. A dietitian can help review your food diary and suggest next steps.
Who should follow the low FODMAP diet and is it right for everyone?
The low FODMAP diet is specifically designed for people with diagnosed IBS, SIBO (small intestinal bacterial overgrowth), or functional digestive disorders. It’s a therapeutic approach that works best when you’ve received proper medical evaluation to rule out other conditions.
This diet isn’t appropriate for everyone. People without digestive symptoms shouldn’t follow it, as unnecessarily restricting FODMAPs offers no health benefits and may reduce beneficial gut bacteria. Children should only follow this diet under professional guidance, as their nutritional needs are different from adults.
Working with a qualified dietitian is highly recommended, especially during the reintroduction phase. They can ensure you maintain proper nutrition, interpret your symptom responses accurately, and avoid unnecessary long-term restrictions.
The low FODMAP diet is a diagnostic and management tool, not a wellness trend or weight-loss plan. It’s meant to improve quality of life for people whose digestive symptoms genuinely interfere with daily activities. If you’re considering this approach, start with a proper IBS diagnosis from your doctor.
What are the common mistakes people make when starting the low FODMAP diet?
Staying on the elimination phase too long is one of the most frequent mistakes. This phase should last only 2 to 6 weeks, yet some people continue eliminating foods for months or even years. This unnecessarily restricts your diet and may reduce beneficial gut bacteria diversity.
Many people eliminate foods that aren’t actually high in FODMAPs, creating unnecessary restrictions. Others don’t properly reintroduce foods, missing the opportunity to identify which specific FODMAPs they can tolerate. The reintroduction phase is crucial but often skipped or done incorrectly.
Assuming you must follow the diet strictly forever is another common misconception. The goal is to identify your personal triggers and then eat the most varied diet possible whilst managing symptoms. Most people can reintroduce many FODMAPs in moderate amounts.
Not working with a qualified dietitian often leads to nutritional gaps, confusion about food choices, and difficulty interpreting symptoms during reintroduction. Professional guidance helps you avoid these pitfalls and achieve better long-term outcomes whilst maintaining a balanced, enjoyable diet. For more detailed information, read our complete guide to the low FODMAP diet.
This article is for informational purposes only and is not medical or dietary advice. Please consult a healthcare professional before making any changes to your diet.