When to Avoid the Low FODMAP Diet

The low FODMAP diet isn’t safe for everyone. While it helps many IBS sufferers, this restrictive protocol can create serious health risks for people with eating disorders, pregnant women, underweight individuals, and children. Certain medical conditions require different approaches, and nutritional needs sometimes outweigh digestive benefits. Recognizing warning signs like worsening symptoms, unintended weight loss, food anxiety, or social isolation helps determine when to stop. Professional guidance ensures proper diagnosis and personalized alternatives like modified FODMAP approaches, gut-directed hypnotherapy, or stress management techniques that address symptoms without extensive restrictions.
Who Should Try the Low FODMAP Diet?

The low FODMAP diet isn’t for everyone—it’s a therapeutic approach designed for specific digestive conditions like IBS and SIBO. Research shows 70% of IBS patients experience symptom improvement, but proper diagnosis is essential before starting. This comprehensive guide explores who should consider the diet, what symptoms indicate FODMAP sensitivity, when to avoid this approach, and how to prepare before beginning. Learn whether this structured three-phase elimination plan could provide the digestive relief you’ve been seeking.
How Long Until Low FODMAP Works?

The low FODMAP diet typically starts working within 2 to 6 weeks, but symptom relief follows a predictable pattern. Bloating and gas often improve within the first two weeks, while bowel habit changes may take longer to normalize. Understanding this timeline helps you stay motivated during the elimination phase and recognize progress. Individual factors like symptom severity, diet adherence, and IBS type all influence how quickly you’ll see results. Learn what symptoms improve first, why some people experience delays, and when to transition to the reintroduction phase for lasting relief.
Low FODMAP Diet Success Rates

Living with IBS and wondering if the low FODMAP diet actually works? Clinical research shows 50-86% of IBS patients experience significant symptom relief, with approximately 70% achieving meaningful improvement. Success depends on proper implementation, professional guidance, and systematic reintroduction. This comprehensive guide explores proven success rates across different IBS subtypes, key factors that influence outcomes, common mistakes that reduce effectiveness, and practical strategies to maximize your results. Discover what the research reveals about long-term adherence and quality of life improvements.
How Low FODMAP Relieves Symptoms

Living with IBS means dealing with bloating, cramping, and unpredictable bowel movements that make every meal stressful. The low FODMAP diet offers scientifically proven relief for 70-80% of IBS sufferers by reducing fermentable carbohydrates that trigger symptoms. Through a structured three-phase process of elimination, reintroduction, and personalization, you’ll identify your specific food triggers while calming digestive distress. Most people notice significant improvements within two weeks, with bloating and gas responding quickest. This isn’t about permanent restriction—it’s an investigative approach to discover what your body tolerates, giving you freedom and lasting symptom control.
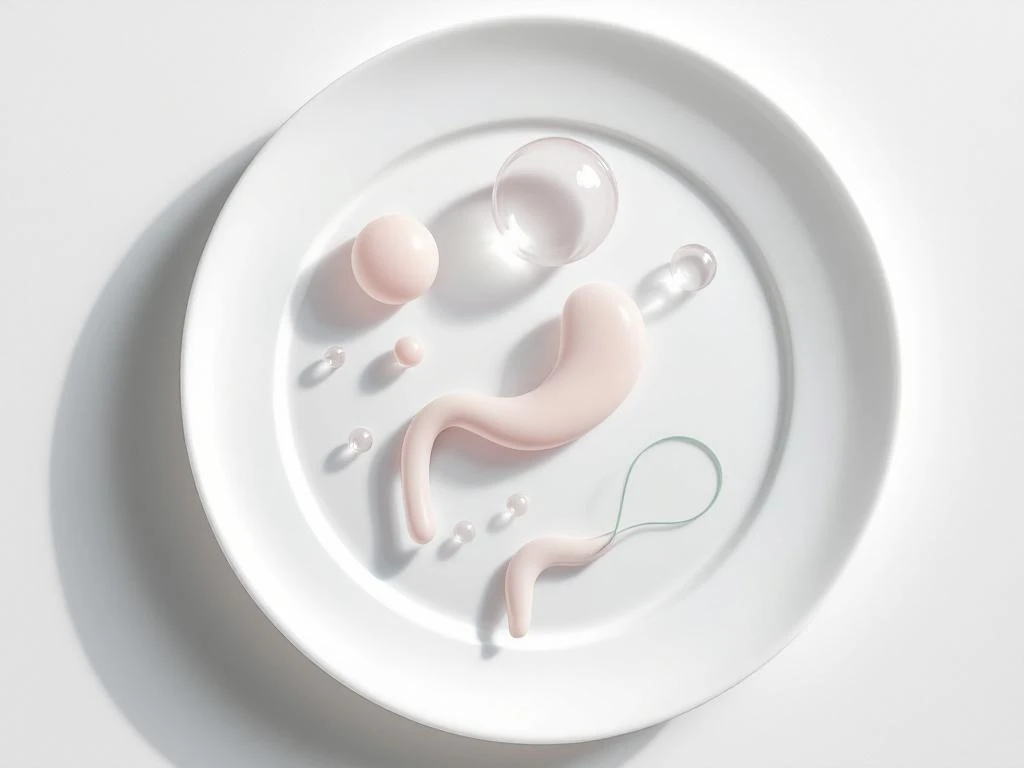
Low FODMAP Impact on Digestive System

Living with IBS and digestive discomfort doesn’t have to control your life. The low FODMAP approach offers science-backed relief by reducing gas production, normalizing bowel movements, and decreasing intestinal inflammation. This comprehensive guide explains the physiological changes that occur during each phase—from elimination through personalized reintroduction—and why following the structured process protects your gut microbiome whilst eliminating uncomfortable symptoms. Learn how strategic FODMAP restriction transforms digestive health without compromising long-term wellness.
What foods are hard to digest?

Some foods are harder to digest than others due to their composition and how they interact with your system. High-fat foods, processed items, artificial sweeteners, raw cruciferous vegetables, dairy products, and fried foods commonly cause digestive discomfort like bloating and gas. Understanding which foods challenge your digestion—including FODMAPs—and implementing strategies like smaller portions, thorough chewing, and proper cooking methods helps you make informed choices for better digestive comfort and overall wellbeing.
Osmotic Effects of FODMAPs Explained

Ever wonder why certain foods cause bloating and urgent bathroom trips? FODMAPs are poorly absorbed carbohydrates that create osmotic pressure in your gut, drawing excess water into your intestines. This water retention causes the distension, cramping, and diarrhea that plague IBS sufferers. Understanding this scientific mechanism reveals why the low FODMAP diet works so effectively—it removes the dietary triggers that create fluid imbalance. Learn which FODMAPs have the strongest osmotic effects, how your body responds to these unabsorbed carbohydrates, and why managing your intake can transform your digestive comfort.
FODMAPs and Gut Microbiome: The Connection

Ever wondered why certain foods trigger digestive discomfort while others don’t? The answer lies in the fascinating relationship between FODMAPs—specific carbohydrates that resist digestion—and the trillions of bacteria in your gut. When FODMAPs reach your colon, gut bacteria ferment them, producing gas and short-chain fatty acids. For people with IBS, this natural process triggers amplified symptoms due to visceral hypersensitivity. Understanding this connection empowers you to manage symptoms effectively while maintaining a healthy microbiome. Discover how the low FODMAP diet works as a three-phase process, not a permanent restriction, and learn practical strategies to support both immediate comfort and long-term gut health.
Why FODMAPs Cause Gas and Bloating
Ever wonder why certain foods leave you bloated and gassy? FODMAPs—poorly absorbed carbohydrates found in wheat, dairy, and many fruits—trigger digestive distress through two key mechanisms: bacterial fermentation that produces gas, and osmotic effects that draw water into your intestines. Understanding these biological processes and identifying your personal triggers through systematic testing can help you regain digestive comfort. Learn the science behind FODMAP intolerance, why some people are more sensitive, and how to determine if FODMAPs are causing your symptoms.
