Coconut Yogurt Berry Bowl

Starting your day with a coconut yogurt berry bowl means choosing a breakfast that’s gentle on your digestive system whilst delivering nutrition and flavour. This beginner-friendly low FODMAP recipe takes just 5 minutes to prepare and requires no cooking skills. Using dairy-free coconut yogurt, safe portions of strawberries and blueberries, and gut-friendly toppings like pumpkin seeds, you’ll create a satisfying breakfast that supports digestive health during any phase of the low FODMAP diet.
How to make low fodmap fried rice
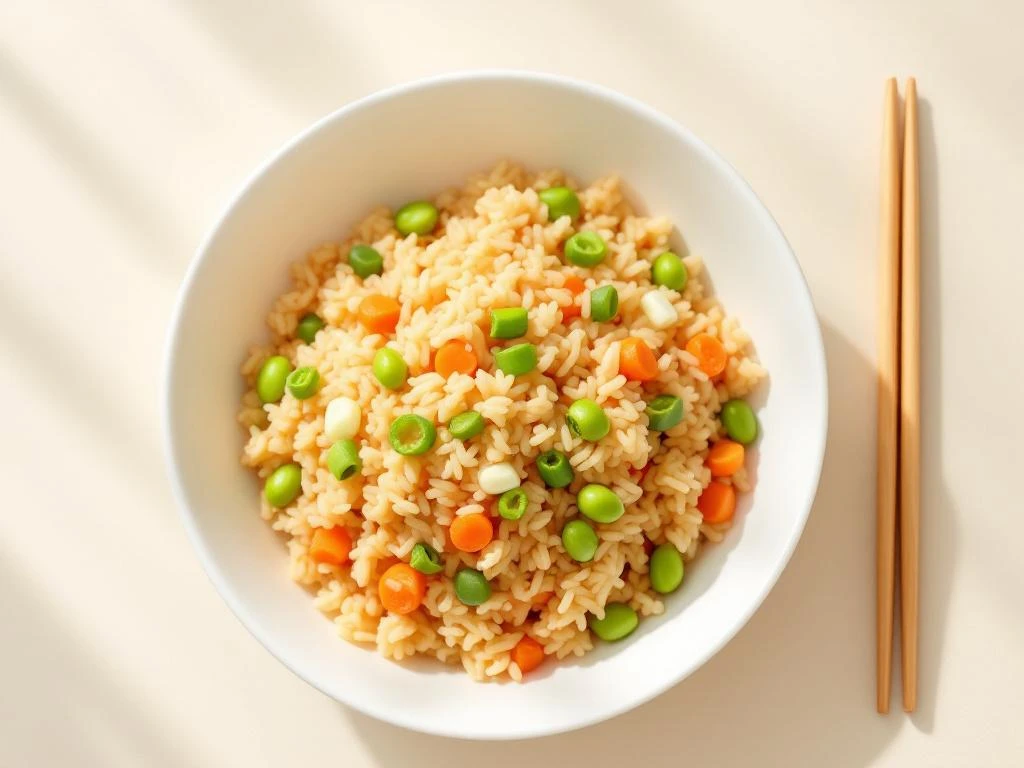
Making low FODMAP fried rice gives you a satisfying, flavourful meal without triggering IBS symptoms. This beginner-friendly recipe swaps out garlic, onion, and wheat-based soy sauce for gut-friendly alternatives like garlic-infused oil, spring onion greens, and gluten-free tamari. Ready in just 30 minutes with day-old rice, you’ll master restaurant-quality texture using simple techniques and safe vegetables. Discover how to enjoy authentic takeaway taste while managing your digestive health—no compromise on flavour required.
How FODMAP Fermentation Affects Your Gut

Ever feel bloated after eating certain foods? FODMAP fermentation might be the culprit. When gut bacteria break down poorly absorbed carbohydrates, they produce gases and draw water into your intestines—creating the perfect storm for IBS symptoms. This natural digestive process affects everyone differently, but understanding how FODMAPs ferment in your colon, why some people experience severe reactions, and which specific foods trigger your symptoms can transform your digestive health. Learn the science behind fermentation and discover practical strategies to identify your personal triggers and manage uncomfortable symptoms effectively.
History of Low FODMAP Diet Development

Discover the fascinating journey behind the low FODMAP diet’s development, from early observations about carbohydrate malabsorption to a globally recognized therapeutic approach for IBS. Learn how Professor Peter Gibson and Dr. Sue Shepherd at Monash University pioneered this evidence-based protocol, transforming digestive health management for millions worldwide. This comprehensive history explores the scientific breakthroughs, clinical refinements, and ongoing evolution that made the FODMAP diet one of the most significant advances in nutritional science for gastrointestinal health.
Dr. Sue Shepherd: Low FODMAP Diet Creator

Meet Dr. Sue Shepherd, the Australian dietitian and researcher who revolutionized IBS management through her groundbreaking discovery of the low FODMAP diet. Through meticulous scientific investigation at Monash University, she identified how fermentable carbohydrates trigger digestive distress and created a systematic, evidence-based approach that has helped millions worldwide. Learn how her unique combination of rigorous research and clinical empathy transformed IBS treatment from guesswork into a personalized, scientifically-valid dietary framework you can apply to your own digestive health journey.
Monash University FODMAP Research

Struggling with IBS and confused about FODMAP advice? The low FODMAP diet isn’t a wellness trend—it’s rigorously tested science from Monash University researchers who identified specific fermentable carbohydrates triggering digestive symptoms. Discover how Monash became the gold standard authority through laboratory testing of hundreds of foods, why their certification programme protects you from misleading claims, and how their continuously updated app provides evidence-based guidance. Understanding this research helps you distinguish reliable information from misinformation and manage symptoms with confidence.
How Does the Low FODMAP Diet Work?
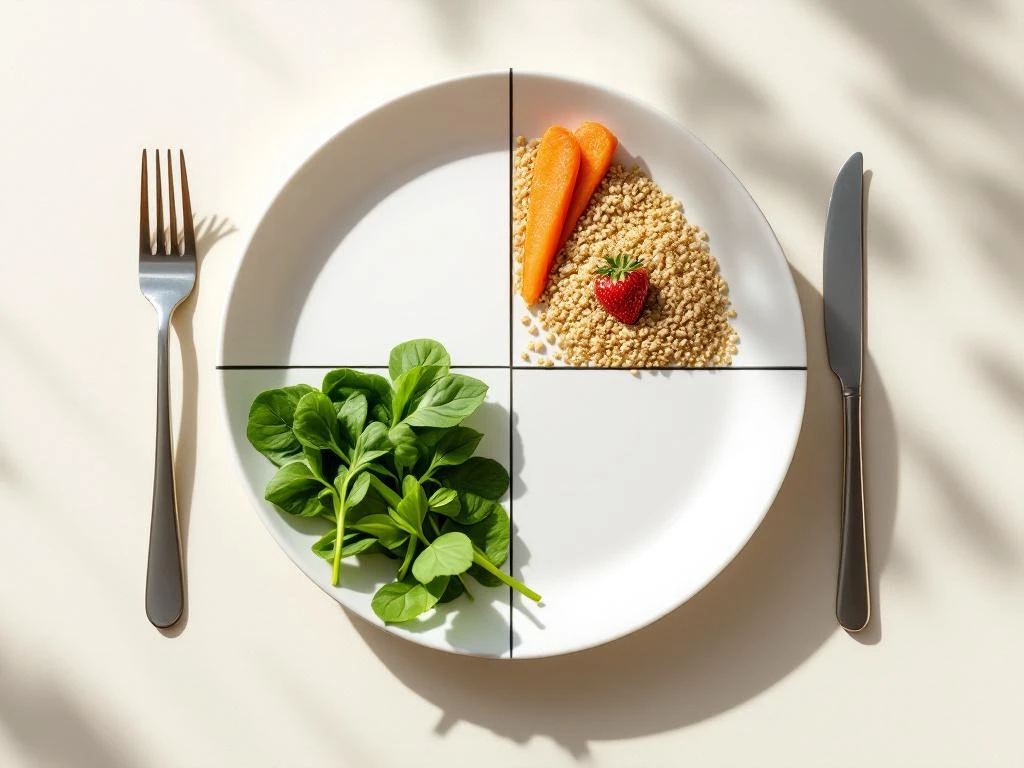
The low FODMAP diet reduces fermentable carbohydrates that trigger IBS symptoms like bloating and pain. Developed by Monash University researchers, this three-phase approach helps identify personal food triggers through elimination, systematic reintroduction, and personalization. Most people see improvement within 2-6 weeks. The diet targets specific carbohydrates that cause osmotic effects and fermentation in sensitive digestive systems, offering a science-based path to managing symptoms whilst maintaining nutritional balance and food variety.
Conditions That Benefit from Low FODMAP

Struggling with digestive discomfort? The low FODMAP diet has proven transformative for specific conditions including IBS, SIBO, inflammatory bowel disease during remission, and even endometriosis-related symptoms. This evidence-based approach works by reducing fermentable carbohydrates that trigger bloating, pain, and altered bowel habits in sensitive individuals. Rather than a permanent restriction, it serves as a diagnostic tool to identify your personal triggers through systematic elimination and reintroduction phases. Understanding whether your condition responds to low FODMAP can be the difference between ongoing discomfort and genuine symptom relief.
Low FODMAP Diet Contraindications
The low FODMAP diet effectively manages IBS symptoms for many, but it’s not suitable for everyone. Certain medical conditions, life stages, and circumstances make this restrictive approach risky or inappropriate. From eating disorder history to pregnancy, nutritional deficiencies to complex health conditions, understanding contraindications protects your wellbeing. This guide examines who should avoid FODMAP elimination, the nutritional risks of long-term restriction, when professional supervision is essential, and safe alternatives for managing digestive symptoms without unnecessary dietary restriction.
Medical Supervision for Low FODMAP Diet

Starting a low-FODMAP diet without professional guidance can lead to nutritional deficiencies, unnecessary restrictions, and missed diagnoses. This therapeutic three-phase diet requires expert oversight from gastroenterologists and specialized dietitians who ensure safe elimination, systematic reintroduction, and personalized long-term plans. Discover why professional supervision transforms this complex dietary approach from guesswork into evidence-based symptom relief while protecting your nutritional health and preventing common pitfalls that derail self-guided attempts.
